UBC researchers invent a synthetic ‘glue’ for blood clots
July 15, 2016
July 15, 2016
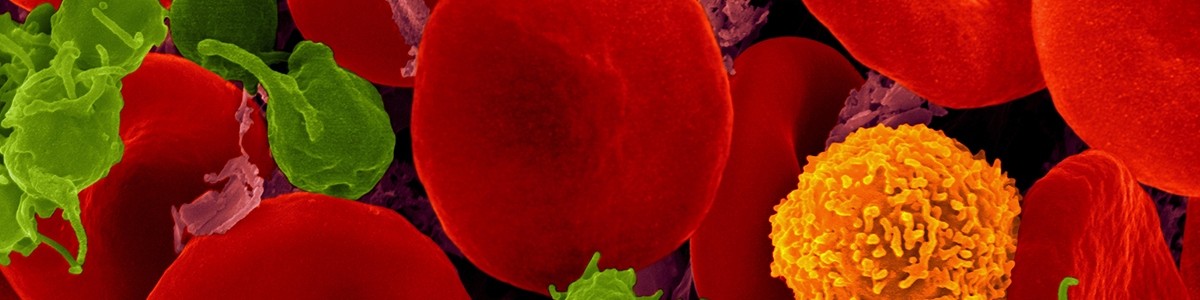
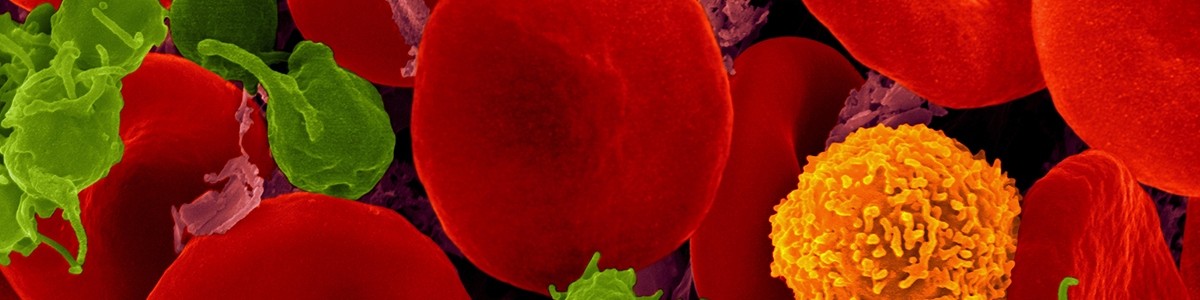
UBC Science graduate student Karen Chan and biochemical engineer Christian Kastrup have developed a synthetic version of fibrin, opening up new possibilities for shoring up blood clots and helping internal wounds heal.
Kastrup and Chan have created a polymer – a large, star-shaped molecule with eight branches. The end of each branch contains a peptide (a small protein) that reacts with a blood enzyme called Factor XIII.
The resulting reactions cause the polymers to link up with each other. The formerly disconnected polymers become less soluble and more solid – in the same way that fibrin, a protein in the blood, congeals to form a clot.
Often, a person’s fibrin isn’t sufficient to keep a clot in place, either because an injury is so large that there simply isn’t enough fibrin, or because fibrinolysis – the body’s natural process of breaking down blood clots – kicks in too early, before a wound has a chance to close.
“Usually it’s a good thing to clear out clots, but in severe trauma, you’re most concerned about stopping the bleeding,” says Kastrup, a scientist in UBC’s Michael Smith Laboratories and Centre for Blood Research. “Sometimes the body is degrading a clot instead of trying to preserve or strengthen it.”
Natural fibrin from donated blood is given to patients with major bleeding, but even supplementary fibrin can be degraded by fibrinolysis. It’s also expensive to produce.
The synthetic fibrin would not be a substitute for natural fibrin, but act as a supplementary “glue” that helps hold a clot together, withstanding both fibrinolysis and the force of blood pressure, and helping to pull a wound closed.
Kastrup and Chan, a PhD candidate in the Genome Science and Technology program, measured the adhesiveness of their polymer on segments of animal blood vessels, and found that it is more than twice as adhesive as a normal clot. The next steps will be to make the polymer more soluble so that it can easily travel through the bloodstream, and then test it in animals.
“But we also might be able to ‘freeze-dry’ the polymer, so that it can be made into sheets and placed on an external wound,” Chan says. “When it comes into contact with blood, it would form a gel and begin reacting with Factor XIII.”
We honour xwməθkwəy̓ əm (Musqueam) on whose ancestral, unceded territory UBC Vancouver is situated. UBC Science is committed to building meaningful relationships with Indigenous peoples so we can advance Reconciliation and ensure traditional ways of knowing enrich our teaching and research.
Learn more: Musqueam First Nation